Hair Loss Evaluation Dallas
Types of Hair Loss Evaluation
 History
History
Experiencing hair loss can be a traumatic experience for anyone. Helping to find out what may be the root cause is important in trying to help identify and thereby treat the condition. Taking a careful history of the prospective patient can be the starting point in evaluation.
Understanding the pattern and duration of hair loss can be instructive. Hair loss that began in childhood may be hereditary or have genetic influences that should be explored. Focal versus diffuse hair loss patterns may indicate different disease processes. For example, a focal area of loss could point toward alopecia areata, a localized tinea capitis, or trichotillomania. Diffuse loss may point toward a telogen effluvium, anagen effluvium or androgenetic alopecia.
Another important distinction concerns whether the person is shedding hair or simply showing thinning of hair. For example, alopecia areata and telogen effluvium are characterized by active hair shedding, whereas androgenetic alopecia is typically a condition of progressive hair thinning. If the hair is shedding, questions that could elicit a positive history of telogen effluvium would include a recent fever, recent anesthesia, pregnancy, crash diet, etc. (See the section on telogen effluvium for more details.) For a female, if the hair is simply thinning, other questions should be asked regarding thyroid abnormalities, irregular menses, or iron deficiency.
If the hair is shedding, a further refining question would be whether the hair is coming out by the roots or showing signs of abnormal breakage. Hairs that fall out by the root might point toward telogen effluvium or androgenetic alopecia. Conversely, hair breakage could arise due to harsh chemical treatments/hair-care products or some kind of anagen effluvium, such as following chemotherapy for cancer. Infections like tinea capitis or other conditions that cause structural hair shaft defects can also lead to abnormal hair breakage.
Clinical Hair Loss Evaluation
After a careful history is taken from the patient, an attentive physical examination should be undertaken of the scalp and hair. In non-scarring alopecias, the area of hair loss will still maintain visible follicular units, whereas with scalp scarring the area of hair loss will have no follicular units and also may have associated appearance of scarring, scaling, and associated redness.
The pattern and distribution of the hair loss may also be instructive. For example, alopecia areata will be random in distribution, whereas androgenetic alopecia (male pattern baldness) will have a distinct and known pattern. Evaluation of the hair shaft may also prove to be helpful to determine the caliber, fragility, length, and shape. Using a contrast sheet of paper to evaluate the hair against a white background can also improve one’s ability to read the hair characteristics.
 Pull Test
Pull Test
A pull test can be administered in which approximately 60 hairs are grasped between the thumb, forefinger, and middle finger and gently tugged. Greater than 10% of hairs that are released indicates an abnormal pull test. Of note, the individual should not shower for at least one day prior to the pull test. Generally speaking, a pull test will help remove the telogen hairs but not normal anagen hairs. Excessive number of telogen hairs may indicate telogen effluvium. Abnormal anagen hairs can also be pulled out, as with loose anagen syndrome or with dystrophic and fragile anagen hairs. Usually, these fragile anagen hair shafts will break somewhere along the shaft and not show any roots. The pulled hairs can then be evaluated on a glass slide under a microscope. Telogen hairs reveal the classic club-shaped and semi-transparent root as distinct from anagen hairs.
Pluck Test- (Trichogram)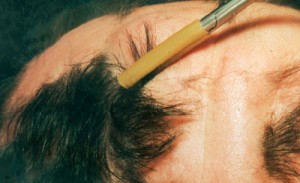
A trichogram or pluck test requires the use of a hemostat with a rubberized end in which 60 to 80 hairs are firmly grasped and forcefully (unlike a pull test) plucked, twisted, and lifted out of the scalp. Hairs shafts are then cut 1 cm above the root, and the roots are evaluated on a slide side by side. Anagen hairs are distinguished from telogen hairs and anagen/telogen ratios are established. Unfortunately, the forceful tug of the anagen hairs will most likely show artefactual changes so that dystrophic or damaged anagen hairs should not be considered pathologic but a result of their forceful removal. For these reasons (and the discomfort involved), the trichogram is rarely used today. A scalp biopsy provides much more information than a pluck test can afford.
 Scalp Counts
Scalp Counts
Daily scalp counts can also be helpful (albeit time consuming). Normal, physiologic hair loss should be approximately 100 to 150 hairs per day. The shed hairs are collected from brushes, sinks, and the shower and placed daily into separate plastic bags. Days in which showering occurs should be noted, as increased shedding is expected on those days. This process should span a 7-day period. Someone losing fewer than 100 hairs per day may be considered to have no active shedding. This process can be repeated at intervals so that the individual can determine progress or worsening of hair shedding.
Scalp Biopsy
A scalp biopsy can be a very informative procedure in which a biopsy of 4mm wide and 4 mm deep is undertaken in an area of active hair loss, like the periphery of an active lesion of alopecia areata. Originally, the biopsy was sectioned vertically to evaluate the longitudinal nature of each hair shaft but today the thought is that a transverse or horizontal section can be more informative in terms of how the hair shafts relate to one another and the anagen to telogen ratios can be better understood. The biopsy is sectioned horizontally to evaluate the upper level at the papillary dermis, at the mid-level at the reticular dermis, and in the deeper levels at the subcutaneous fat. The upper levels typically contain all telogen and anagen hairs as well as terminal and vellus hairs. The mid-levels contain the anagen and telogen hairs but only terminal hairs. The deep levels only contain anagen and terminal hairs. Therefore, anagen/telogen ratios and terminal/vellus hair ratios can be calculated with horizontal sectioning.
Associated laboratory work up can also be helpful such as serum ferritin to rule out iron deficiency anemia as a cause of hair loss, particularly in women with a diffuse patterned hair loss. Thyroid function tests, specifically thyroid-stimulating hormone (TSH), may be required as part of a thorough work up. Any virilizing signs in women including irregular menses, hirsutism, or acne should be evaluated with both free testosterone and dehydroepiandrosterone sulfate (DHEAS). When lupus is suspected, a serum antinuclear antibody (ANA) will be important.




